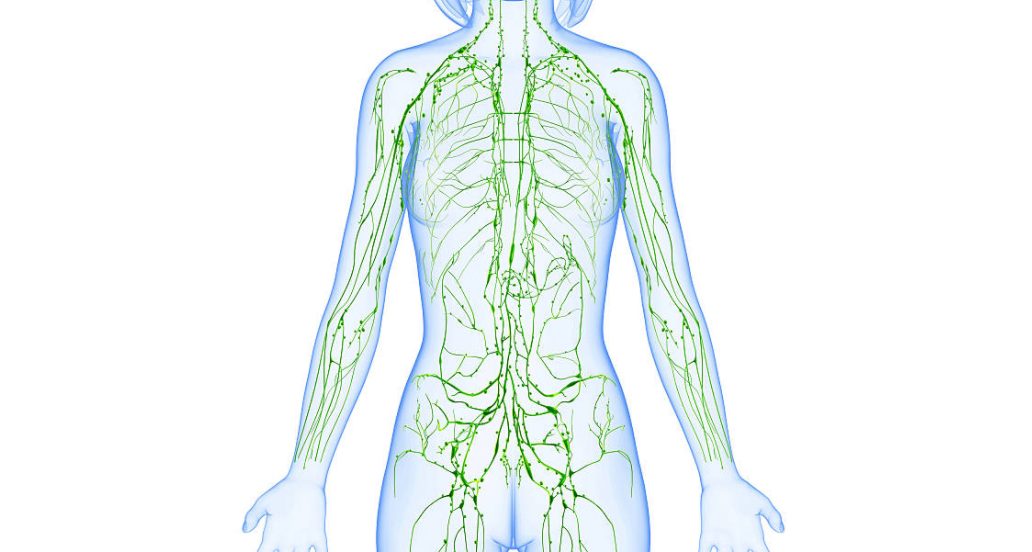
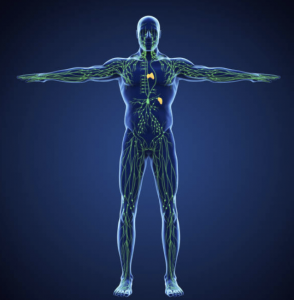
The lymphatic system is part of our immune system, and is crucial to keeping the body healthy.
It contains a network of lymph nodes and lymph vessels that collect and carry watery, clear lymph fluid throughout your body, collecting bacteria, viruses and waste products.
When these vessels are blocked or unable to carry lymph fluid away from the tissues, localised swelling to the arm or leg can occur. This is called lymphedema.
What causes lymphedema?
Lymphedema can be either primary or secondary. This means it can occur on its own (primary lymphedema) or it can be caused by another disease or condition (secondary lymphedema).
Primary lymphedema is present at birth due to inherited conditions in which lymph nodes or vessels are absent or abnormal, such as:
- Milroy’s disease (congenital lymphedema): This disorder begins in infancy and causes lymph nodes to form abnormally.
- Meige’s disease (lymphedema praecox): This disorder often causes lymphedema around puberty or during pregnancy, though it can occur later, until age 35.
- Late-onset lymphedema (lymphedema tarda): This occurs rarely and usually begins after age 35.
Secondary lymphedema is far more common than primary lymphedema. Secondary lymphedema develops as a result of damage to or dysfunction of the lymphatic system. This can be due to any form of trauma such as:
- Cancer – cancer cells can block lymphatic vessels
- Infection – infection of the lymph nodes or parasites can restrict the flow of lymph fluid
- Scar tissue – caused by radiation therapy or surgical removal of lymph nodes
Lymphedema is most commonly caused by the removal of or damage to your lymph nodes as a part of cancer treatment, particularly breast cancer, due to the surgical removal of lymph nodes and/or radiation treatment that can change the flow of lymph fluid in that part of the body.
Signs & Symptoms

Signs and symptoms of lymphedema can include:
- Swelling in the breast, chest, shoulder, arm, or hand
- Part of your body feeling full or heavy
- Skin changing texture, feeling tight or hard, or looking red
- New aching, tingling, or other discomfort in the area
- Less movement or flexibility in nearby joints, such as your shoulder, hand, or wrist
- Trouble fitting your arm into jacket or shirt sleeves
- Your bra not fitting as well as it used to
- Your ring, watch, and/or bracelet feeling tight, and you haven’t gained weight
- A decreased ability to see or feel the veins or tendons in the extremities
- Asymmetrical appearance of the extremities
Early on, the skin usually stays soft, and raising your affected arm might relieve the swelling. However, over time, the swollen area may become hot and red and the skin hard and stiff.
To diagnose the condition, your doctor may order imaging tests to get a look at your lymph system. Tests may include:
- MRI scan: Using a magnetic field and radio waves, an MRI produces 3-D, high-resolution images.
- CT scan: This X-ray technique produces detailed, cross-sectional images of your body’s structures. CT scans can reveal blockages in the lymphatic system.
- Doppler ultrasound: This variation of the conventional ultrasound looks at blood flow and pressure by bouncing high-frequency sound waves (ultrasound) off red blood cells. Ultrasound can help find obstructions.
- Radionuclide imaging of your lymphatic system (lymphoscintigraphy): During this test you’re injected with a radioactive dye and then scanned by a machine. The resulting images show the dye moving through your lymph vessels, highlighting blockages.
Lymphedema: What to Expect?
 There is no way to predict who will develop lymphedema. However, factors that may increase your risk of developing lymphedema after cancer, cancer treatment or other secondary causes include:
There is no way to predict who will develop lymphedema. However, factors that may increase your risk of developing lymphedema after cancer, cancer treatment or other secondary causes include:
- Older age
- Excess weight or obesity
- Rheumatoid or psoriatic arthritis
In most cases, lymphedema develops slowly over time. The swelling can range from mild to severe. It can start soon after surgery and/or radiation treatment, but can also occur months or even years later.
Lymphedema can lead to serious complications, such as:
- Infections that can result from lymphedema include a serious bacterial infection of the skin (cellulitis) and an infection of the lymph vessels (lymphangitis). The smallest injury to your arm or leg can be an entry point for infection.
- Lymphangiosarcoma, a rare form of soft tissue cancer can result from the most severe cases of untreated lymphedema. Possible signs of lymphangiosarcoma include blue-red or purple marks on the skin. This is an aggressive cancer that is treated by amputation of the affected limb. Even with treatment, the prognosis is poor.
- Deep venous thrombosis (formation of blood clots in the deeper veins) is also a known complication of lymphedema.
- Impairment of functioning in the affected area and cosmetic issues are further complications of lymphedema.
Treatment for Lymphedema

There is no cure for lymphedema; however it can be managed with early diagnosis and care of the affected limb. Treatment approaches include:
- Wrapping your arm or leg
Bandaging your entire limb encourages lymph fluid to flow back toward the trunk of your body. The bandage should be tightest around your fingers or toes and loosen as it moves up your arm or leg. A lymphedema therapist can show you how to wrap your limb.
- Exercises
Light exercises in which you move your affected limb may encourage lymph fluid drainage and help prepare you for everyday tasks, such as carrying groceries. Exercises shouldn’t be strenuous or tire you but should focus on gentle contraction of the muscles in your arm or leg. A certified lymphedema therapist can teach you exercises that may help.
- Pneumatic compression
A sleeve worn over your affected arm or leg connects to a pump that intermittently inflates the sleeve, putting pressure on your limb and moving lymph fluid away from your fingers or toes.
- Compression garments
Long sleeves or stockings made to compress your arm or leg encourage the flow of the lymph fluid out of your affected limb. Obtain a correct fit for your compression garment by getting professional help.
- Massage
A special massage technique called manual lymph drainage may encourage the flow of lymph fluid out of your arm or leg. Be sure to have it done by someone specially trained in the technique. Massage isn’t for everyone. Avoid massage if you have a skin infection, active cancer, blood clots or congestive heart failure. Also avoid massage on areas of your body that have received radiation therapy.
- Complete decongestive therapy (CDT)
This approach involves combining therapies with lifestyle changes. Generally, CDT isn’t recommended for people who have high blood pressure, diabetes, paralysis, heart failure, blood clots or acute infections.
In cases of severe lymphedema, your doctor may consider surgery to remove excess tissue in your arm or leg to reduce swelling.
Research advances have led to procedures like sentinel lymph node biopsy, which allows the surgeon to remove fewer lymph nodes.
Studies are also looking at ways to find the lymph nodes that drain the arm before surgery so they can be saved when possible. This is called axillary reverse mapping.
Living with Lymphedema

Your certified lymphedema therapist will discuss a comprehensive course of therapy to adopt lifelong measures. Here are some general tips to observe if you have lymphedema:
- Get regular medical check-ups
Regular check-ups should include checking for lymphedema. If you’ve been recording arm and leg measurements, this may be part of the check-up.
- Try to get to and/or stay at a healthy weight
Obesity is known to be a major risk factor for lymphedema. A person with lymphedema should maintain a normal body weight and seek professional help to lose weight if your weight is above standard recommended guidelines.
- Exercise
It’s important to use your affected arm for normal, everyday activities to help you heal properly and regain strength. This includes doing things like brushing your hair and bathing. Using your muscles helps drain lymph fluid from your arms. It also helps keep your muscles flexible and helps reduce scarring.
- Use of compression garments
Compression garments are fitted sleeves that can help control lymphedema. They can help prevent or reduce swelling by moving lymph fluid from the arm back into the body. Careful fitting is needed, and you should follow your health care professional’s advice on use and care of the garment.
- Maintain good hygiene and skin care
- Have your blood drawn, blood pressure taken, IVs, vaccinations and shots done in your unaffected arm or another location, if you can.
- Keep your hands and cuticles soft and moist by regularly using moisturising lotion or cream
- Clean and protect any skin breaks caused by cuts, scratches, insect bites, hangnails, or torn cuticles.
- Wear protective gloves with sleeves when doing household chores that use harsh chemical cleansers or steel wool, when gardening or doing yard work, and when working with animals that might scratch or bite.
- Wear a thimble when sewing to cut down on needle and pin pricks to your fingers.
- Be extra careful when shaving your underarms, and use a clean razor on clean skin.
- Use an insect repellent to help prevent bug bites when outdoors. If you’re bit or stung on the affected arm, clean and put ice on the area and raise the arm.
- Try to avoid burns, including sunburns, and extreme temperatures.
- Use oven mitts that cover your lower arms. Be careful when frying foods, boiling liquids, and removing food from a microwave oven.
- Avoid adding pressure to the affected limb
- Wear loose jewelry, clothing, bras, and gloves.
- Avoid anything that fits too tightly or puts pressure around your chest, arm, or wrist.
- Be sure compression garments fit well and are worn properly. Clothing and compression garments should be supportive and have smooth, even compression.
- Do not use shoulder straps when carrying briefcases and purses.
- Wear a loose-fitting bra with padded straps that don’t dig into your shoulder.
- Stasis: People with leg lymphedema should avoid conditions which cause stasis. Stasis refers to sitting or standing for a long period of time without moving, changing position, or elevating the legs.
- These general measures can assist you with living with lymphedema. However, it is crucial to seek professional help and guidance from a certified lymphedema therapist, who will work in conjunction with your doctors to provide the best approach to treatment and management of the condition.